Combined Spinal & Epidural Block
Combined Spinal & Epidural Block
Spinal anesthesia is typically used for surgical procedures on the lower body. Epidural anaesthesia, by contrast, involves inserting an epidural needle into the space just outside the spinal cord. This technique reduces or removes pain felt below this level and decreases sensation in these areas.
Description
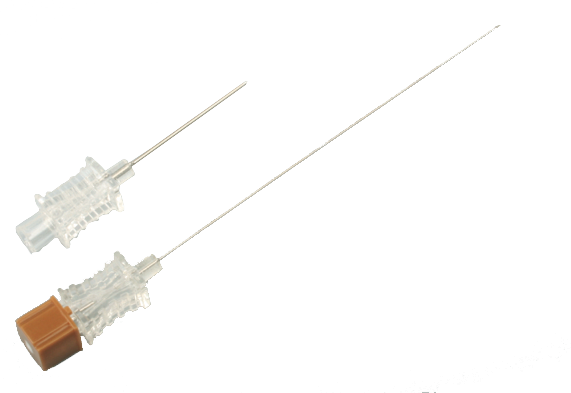
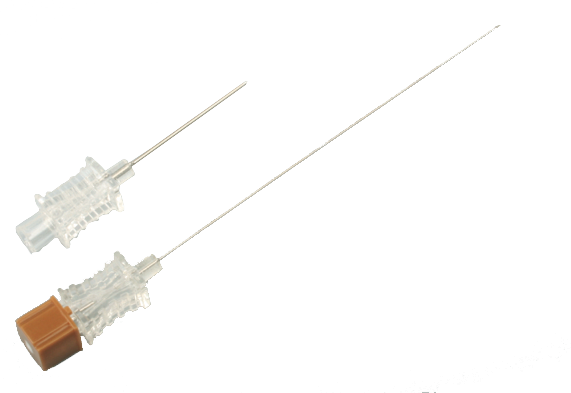
Size: 25G x 110 mm & 16G x 80 mm
- Bleeding the advantages of both atraumatic spinal needle and epidural needle, featuring the excellence of exact effect, significant muscle relaxing effect, small amount of anesthetic for local anaesthesia and no PDPH on the whole.
- Capable of performing continuous epidural anaesthesia following spinal anaesthesia or postoperative pain ease as per clinical requirements.
What is the combined spinal and epidural anaesthesia technique?
The combined spinal and epidural anaesthesia technique is a regional anaesthetic technique that involves the administration of anaesthesia to the spinal cord and nerves as well as the epidural space. This technique provides both surgical and analgesic benefits, and is often used for major surgery such as Cesarean sections, hip replacements, and abdominal surgeries. The main advantage of this technique is that it allows for a more precise delivery of anaesthesia to the target area while sparing other areas of the body from unwanted effects.
Comparisons of CS/EP vs. spinal vs. epidural anaesthesia and analgesia
There are several advantages and disadvantages to each type of regional anaesthesia, and the best option for a given patient depends on many factors. Here, we compare CS/EP with spinal and epidural anaesthesia and analgesia, in terms of their efficacy, side effects, and other important considerations. Efficacy: CS/EP is generally more effective than either spinal or epidural anaesthesia alone, due to the combined effect of the two types of anaesthesia. The main advantage of CS/EP over spinal anaesthesia is that it provides better pain relief during labour and delivery. The main advantage of CS/EP over epidural anaesthesia is that it has a faster onset and provides more reliable pain relief. Side effects: Spinal and epidural anaesthesia can both cause side effects such as hypotension, nausea, and vomiting. CS/EP may also cause these side effects, but they are typically less severe with this technique. Other considerations: In some cases, patients may not be suitable candidates for either spinal or epidural anaesthesia due to medical conditions such as obesity or pregnancy-induced hypertension. In these cases, CS/EP may be the best option.
Spinal, epidural or combined?
There are three main types of regional anaesthesia: spinal, epidural and combined. Combined spinal and epidural anaesthesia (CSEA) is a technique that combines both spinal and epidural anaesthesia to provide anesthesia for surgery. Spinal anaesthesia is when medication is injected into the cerebrospinal fluid (CSF) around the spinal cord to numb the area below the injection site. Epidural anaesthesia is when medication is injected into the space around the spinal cord to numb the area below the injection site. Combined spinal and epidural anaesthesia is a technique that combines both spinal and epidural anaesthesia to provide anesthesia for surgery.
The advantages of CSEA include:
-It provides anesthesia for surgery with less risk of complications than general anesthesia
-It doesn't require intubation or ventilation
-It has a lower incidence of nausea and vomiting than general anesthesia
-It allows for a faster recovery after surgery
-It provides good postoperative pain relief
Combined Spinal Epidural Block
CSE versus Epidural
Epidural anesthesia may be associated with incomplete sensory blockade and poor sacral spread.
4 It however allows for gradual dosing and thus intermittent assessment of completeness of sensory blockade and change in blood pressure. A CSE with a low-dose spinal anesthetic can achieve similarly stable thermodynamics, while reliably producing dense, non-patchy sensory blockade with improved sacral spread when compared to epidural anesthesia alone.
Combined Spinal Epidural Block
One proposed explanation for the improved block following CSE is the phenomenon of local anesthetic flux through the dural puncture site. Suzuki et al.
6 demonstrated enhanced caudal spread of local anesthetic when the dura was punctured with a 26-gauge spinal needle prior to an epidural bolus when compared to patients who received an epidural alone. Other studies demonstrated no detectable flux when 27 or 29-gauge spinal needles were used.
4,7 Case reports have described inadvertent dural puncture from the epidural Tuohy needle resulting in a total spinal secondary to local anesthetic flux. Therefore, the size of the needle used for dural puncture appears to be the primary determinant for the amount, if any, of local anesthetic flux that occurs. Presumably, multiple dural punctures would also increase the amount of flux that occurs.
Another proposed explanation for the improved success rate of the CSE technique is that the spinal needle may aid in correct identification of the epidural space. A spinal needle with adequate CSF return when using a needle-through-needle CSE technique suggests proper placement of the Tuohy needle in the epidural space. Without this confirmation, a false loss of resistance can result in a catheter being placed in area outside the epidural space. A 2005 study by Norris et al. showed a 1.3% of epidural catheters placed with an epidural technique produced no sensory or motor changes and were likely never in the epidural space.8 This same study showed that catheters placed with a CSE technique had a lower incidence of failure than an epidural technique8
A 2005 study by Miro et al.9 in 6497 parturients found a nearly two-fold increase in the catheter replacement rate in patients receiving epidurals compared to the CSE group. However, the disadvantages of CSE cited in this study included higher reported incidences of pruritus, paresthesias, and back pain.
CSE versus Spinal
Spinal anesthesia can cause an abrupt onset of hypotension due to rapid sympathetic blockade. This can be undesirable in patients with limited cardiac reserve or depleted intravascular volume. With a CSE technique, the initial low anesthetic dose administered intrathecally can achieve a rapid onset of block yet the epidural catheter inserted can be used later to ensure an adequate level of sensory blockade, and to prolong the block for surgical anesthesia or post-operative analgesia.
Epidural Volume Extension (EVE)
Proper use of the CSE technique requires an understanding of the interrelationship between the thecal sac and the epidural space. Administration of an epidural fluid bolus may increase pressure in the epidural compartment resulting in compression of the thecal sac. An MRI study revealed that the thecal sac is maximally compressed 5 minutes after an epidural fluid bolus, with effects lasting for up to 30 minutes.10 During CSE, epidural bolus injection and thecal sac compression can lead to enhanced cephalad spread of the spinal anesthetic in the intrathecal space.11 This volume based phenomenon is termed epidural volume extension (EVE), epidural volume expansion, or epidural top-up. Saline or local anesthetic appear to have similar effects on enhanced spinal anesthetic spread.
Timing of the epidural bolus, and local anesthetic baricity further determine the extent of EVE. If the epidural bolus is administered shortly after the spinal dose, intrathecal spread is more pronounced than when it is given more than 20 minutes after the spinal dose.
12 In a study involving male patients undergoing lower extremity surgery, CSE anesthesia performed in the sitting position using isobaric bupivacaine resulted in enhanced cephalad spread following epidural bolus administration but this was not seen with hyperbaric bupivacaine.
13 Other studies, however, have shown cephalad EVE with the use of hyperbaric bupivicaine if the epidural bolus was administered within 5 minutes of the spinal dose.
14
As mentioned earlier, when using 27 or 29-gauge spinal needles, local anesthetic flux from the epidural to subarachnoid space does not appear to contribute to enhanced spinal blockade. This is confirmed by the finding that both block quality and the extent of cephalad spread is the same irrespective of epidural local anesthetic (in low concentrations) or saline bolus injection. Furthermore, 5 mL of saline was noted to be as effective as 10, 15 or 20 mL with regards to enhancing cephalic spread.
15 Block height is typically extended by two to four
dermatologist, EVE is an important phenomena to consider when using the CSE technique, Combined Spinal Epidural Block and explains why an other wise normal dose of spinal anesthetic can result in a high spinal blockade.
The study by Irita et al. examined the incidence of cardiac arrest and death due to improper anesthetic management in patients receiving CSE, spinal, and epidural anesthesia. There is essentially no difference in the cardiac arrest rate and mortality between the CSE and spinal anesthetic groups. Epidural anesthesia, however, was associated with higher cardiac arrest and mortality rates.