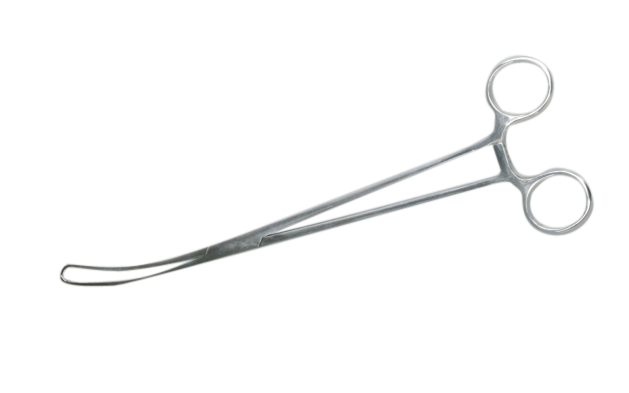
Cervix forceps, During elective (planned) caesarean sections, some obstetricians routinely dilate the cervix intraoperatively, using sponge forceps, a finger, or other instruments, because the cervix of women not in labour may not be dilated, and this may cause obstruction of blood or lochia drainage. However, mechanical cervical dilatation during caesarean section may result in contamination by vaginal micro‐organisms during dilatation, cervix forceps and increase the risk of infection or cervical trauma.
Cervix Forceps
[caption id="" align="alignnone" width="629"]
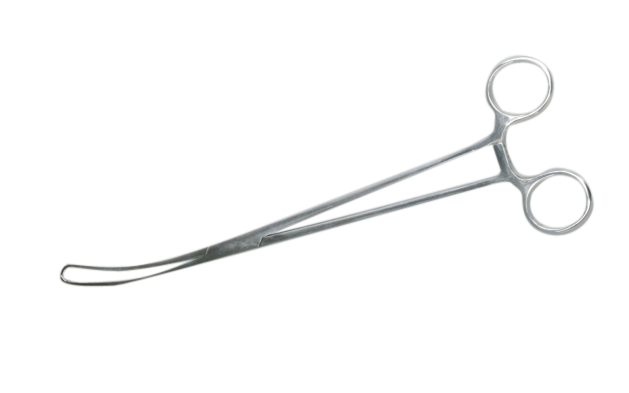
Cervix Forceps[/caption]
Selection criteria
We included all randomised, quasi‐randomised, and cluster‐randomised controlled trials comparing intraoperative cervical dilatation using a finger, sponge forceps, or other instruments during elective caesarean section versus no mechanical dilatation.
Main results
We included eight studies with a total of 2227 women undergoing elective caesarean section. Of these, 1097 underwent intraoperative cervical dilatation with a double‐gloved index finger or Hegar dilator inserted into the cervical canal to dilate, and 1130 did not undergo intraoperative cervical dilatation. Six of the eight included trials had a high risk of bias for some of the risk of bias domains.
Very low‐quality evidence suggested it was unclear whether cervical dilatation had any impact on postpartum haemorrhage (estimated blood loss greater than 1000 mL; risk ratio (RR) 1.97, 95% confidence interval (CI) 0.48 to 8.13; 5/205 versus 3/242; one study, 447 women).
Low‐ or very low‐quality evidence showed no clear difference for the need for blood transfusion (RR 3.54, 95% CI 0.37 to 33.79; two studies, 847 women); postoperative haemoglobin (mean difference (MD ‐0.05, 95% CI ‐0.15 to 0.06; three studies, 749 women), or haematocrit (MD 0.01%, 95% CI ‐0.18 to 0.20; one study, 400 women); the incidence of a drop from baseline haemoglobin above 0.5 g/dL (RR 0.92, 95% CI 0.64 to 1.31; two studies, 722 women), or amount of haemoglobin drop (MD ‐0.01 g/dL, 95% ‐0.14 to 0.13; three studies, 796 women); the incidence of secondary postpartum haemorrhage within six weeks (RR 1.18, 95% CI 0.07 to 18.76; one study, 447 women); febrile morbidity (RR 1.18, 95% CI 0.76 to 1.85; seven studies, 2126 women); endometritis (RR 0.94, 95% CI 0.35 to 2.52; four studies, 1536 women); or uterine subinvolution (RR 0.34, 95% CI 0.08 to 1.36; two studies, 654 women); the results crossed the line of no effect for all of the outcomes. There were no data for cervical trauma.
We found a slight improvement with mechanical dilatation for these secondary outcomes, not prespecified in the protocol: mean blood loss, endometrial cavity thickness, retained products of conception, distortion of uterine incision, and healing ratio. The evidence for these outcomes was based on one or two studies. Cervical dilatation did not have a clear effect on these secondary outcomes, not prespecified in the protocol: wound infection, urinary tract infection, operative time, infectious morbidity, and integrity of uterine scar.