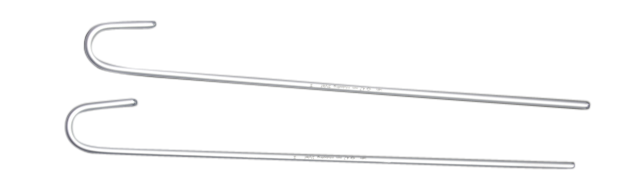
Many people are aware of the intubating stylet, however, they may not be aware of the malleable aluminum covered intubating stylet. This type of stylet is excellent for those who want to avoid the use of a metal tube. It is also more comfortable for the patient and can be reused.
Made of malleable aluminum covered with plastic sheath used for intubation assisatance.
| Ref. No.: | Size: | Applicable ETT: | Length (mm) | Qty. Cs: |
|---|---|---|---|---|
| NMR103001 | 6 FR | <3.5 | 302 | 400 |
| NMR103003 | 10 FR | 4.0-5.0 | 382 | 400 |
| NMR103005 | 14 FR | >5.5 | 382 | 400 |
An intubating stylet is a medical device that is inserted into the trachea (windpipe) through the mouth in order to help place a breathing tube. The intubating stylet is malleable, meaning it can be bent into different shapes. It is also covered in aluminum, which helps it slide more easily through the trachea.
If you need to intubate a patient, you'll need to use an intubating stylet. This guide will show you how to properly use the device.
First, assemble the intubating stylet. You'll need the malleable aluminum covered rod, the distal end cap, and the proximal end cap. Screw the end caps onto the rod, making sure that they are tight.
Next, lubricate the rod with a water-soluble jelly. This will help the rod slide into the patient's trachea more easily.
Now it's time to insert the stylet into the patient. Start by placing the tip of the rod at the entrance of the trachea. Then, gently insert the rod into the trachea until it reaches the vocal cords. At this point, you should be able to see the end of the rod poking through the vocal cords.
Finally, inflate the balloon at the end of the rod. This will help keep the tube in place once it is inserted. Now you can remove the stylet and insert a breathing tube into the patient's trachea.
An intubating stylet is a malleable aluminum covered rod that is used to facilitate the placement of an endotracheal tube. The use of an intubating stylet can help ensure proper placement of the endotracheal tube and minimize the risk of complications associated with intubation. Some of the potential benefits of using an intubating stylet include:
1. Reduced risk of esophageal intubation: One of the most serious complications associated with intubation is esophageal intubation, which occurs when the endotracheal tube is placed into the esophagus instead of the trachea. This can be very dangerous and even life-threatening. The use of an intubating stylet can help reduce the risk of esophageal intubation by ensuring that the endotracheal tube is properly positioned.
2. Reduced risk of airway trauma: Another complication associated with intubation is airway trauma. This can occur when the endotracheal tube is inserted too deeply into the trachea or if it is inserted at an angle that damages the airway tissues. The use of an intubating stylet can
An intubating stylet is a malleable aluminum rod that is used to help place a breathing tube into a patient's airway. While it is a useful tool, there are some risks associated with using an intubating stylet.
One risk is that the aluminum rod can break, which can cause it to become lodged in the patient's airway. Another risk is that the rod can bend, which can make it difficult to remove from the patient's airway. Finally, if the rod is not placed correctly, it can cause the patient's airway to be blocked.